Multiple sclerosis (MS) may progress from the outermost layers of the brain to its deep parts, and isn’t always an “inside-out” process as previously thought, reported a new collaborative study from researchers at the Mayo Clinic and the Cleveland Clinic. The traditional understanding is that the disease begins in the white matter that forms the bulk of the brain’s inside, and extends to involve the brain’s superficial layers, the cortex. Study findings support an opposite, outside-in process: from the cerebrospinal fluid-filled subarachnoid space, that cushions the outside of the brain and the cortex, into the white matter. The new findings will guide researchers as they seek to further understand and treat the disease. The study was published in the December 8th, 20011 issue of the New England Journal of Medicine.
Link to these research findings here
It says 'the early lesions were highly inflammatory'
It has been recognised for some time that some MS cases can be caused by infections such as Chamydia Pneumonia websites here and here
and Lyme Disease.
Microbiologist Thomas Grier has lectured extensively on Lyme disease and Multiple Sclerosis, links to several of his lectures are posted in the right hand column of this blog.
Below was Tom's response to the new MS research :-
The observation that early MS begins with inflammation in the outer cortical regions of the brain seems to fit with the physiology of the location of the BBB and the close proximity to microglia cells, an arrangement that suggests something is crossing the BBB to initiate inflammation and vessel infiltrate.
It is also interesting that white matter lesions later on seem to aggregate around or near the central ventricles often with micro-vessel inflammation/infiltrate seen in the ependyma membrane of the ventricles. This also suggests some outside factor is entering from the “Outside-In” through the CSF.
The spirochete hypothesis of sclerosing pathology suggested by myself, suggests that Borrelia (various species) enter through the BBB and inflame the vessels and activate microglia. Some motile bacteria may also enter the subarachnoid space a place spirochetes cannot thrive and then find their way to the ventricles-ependyma and back into blood vessels where spirochetes can find a more favorable environment. Increases in quinolinic acid levels from BBB-junction inflammation may also contribute to white matter destruction without the direct presence of the bacteria in the white matter lesions. (Spirochetes are more often found in the gray-matter)
This is born out by the lack of spirochetes found in white matter lesions, but classical forms when found, are almost always in the gray matter. This can be seen by using silver stains combined with microwave deflation of the fresh brain cells allowing the spirochetes from many levels becoming visible as the metal coated bacteria rise through the collapsed brain tissue.
This spirochete sclerosing model addresses
1) cortical gray-matter inflammation,
2) rise of an inflammatory toxin of demyelination Quinolinic Acid
3) a mechanism that explains periventricular inflammation and lesions secondary to BBB breakdown and gray-matter inflammation.
4) A possible reason for heterogeneous plagues prevailing
5) The increased incidence of MS in Lyme endemic areas
6) Intracellular infection in neurons explains lack of positive serology tests and patient relapses after antibiotics.
1) cortical gray-matter inflammation,
2) rise of an inflammatory toxin of demyelination Quinolinic Acid
3) a mechanism that explains periventricular inflammation and lesions secondary to BBB breakdown and gray-matter inflammation.
4) A possible reason for heterogeneous plagues prevailing
5) The increased incidence of MS in Lyme endemic areas
6) Intracellular infection in neurons explains lack of positive serology tests and patient relapses after antibiotics.
It seems that if spirochetes play a role in forming some plaques similar to MS plaques, then in order to get good data for treatment research we must consider trying to separate the Spirochete Sclerosing componant from the rest of the data.
For example an immune modulating drug might help true MS but if the data is mixed with patients from Lyme endemic areas that have not been separated in these trials, then treatment may have brief improvement and then a worsening without knowing which patients have an infectious component.
In the hundreds of biopsies used in this study were any also stained with anti-Borrelia antibody fluorescent stains or silver stains? If not we can make no conclusions that spirochetes did not play a role in the gray-matter pathologies.
Tom Grier (A survivor a primary progressive MS)
Earlier this year research by Sam Donta here
SPECT Brain Imaging in Chronic Lyme Disease
Conclusions: Brain SPECT scans are abnormal in most patients with chronic Lyme disease, and these scans can be used to provide objective evidence in support of the clinical diagnosis. The use of certain antibiotic regimens seems to provide improvement in both clinical status and SPECT scans.
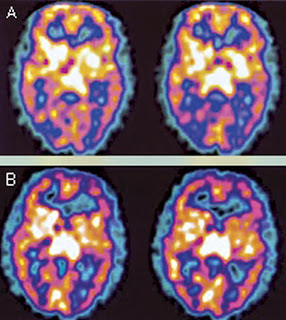
Figure 2
FIGURE 2. SPECT scan of the brain before (A) and after (B) antibiotic treatment. These transaxial images are from a 51-year-old man diagnosed with Lyme disease with a recent change in memory. Representative pretreatment images show hypoperfusion within the mid posterior and mid temporoparietal cortex bilaterally. Representative posttreatment images (14 months later) reveal improved perfusion to the posterior temporoparietal cortex bilaterally, correlating with improved symptoms. Perfusion within the remaining cerebral cortex, basal ganglia, thalamus, and cerebellum was normal.
I think this also goes along way to explaining CCSVI in the MS and Lyme population. There are so many similarities in these two diseases. I have a diagnosis of MS and now Lyme, Bartenella and Babesia along with CCSVI.
ReplyDeleteHi Sean Thanks for your comment I noted that Dr jemsek at ILADS conference discussed cases of Lyme that were having some successes with this process but I got the impression that he had only experience of one clinic and reading between the lines I think care may need to be taken where patients get this procedure done. Good luck with your treatment you have a complex illness of pathogens that you are dealing with but hopefully progress can be made.
ReplyDeleteHi, Joanne, there has been new research and they find that spirochetes seek out lymph nodes and cause neutrophils to proliferate. Neutrophils are white blood cells that get sent by the body to inflamation and infection sites. Wouldn't an infected neutrophil be an ideal spirochete train. It hops on board, and a few minutes later gets sucked up by a tick at a slightly inflamed bite. Or it hops on board and a few days later the neutrophil dies inside brain tissue. I have seen micrographs of infected neutrophils and a friend with Lyme has elevated neutrophil levels. Maybe the lyme even elevates the neutrophil levels to keep down co-infections and give them less competition.
ReplyDelete